Understanding the Distinctions
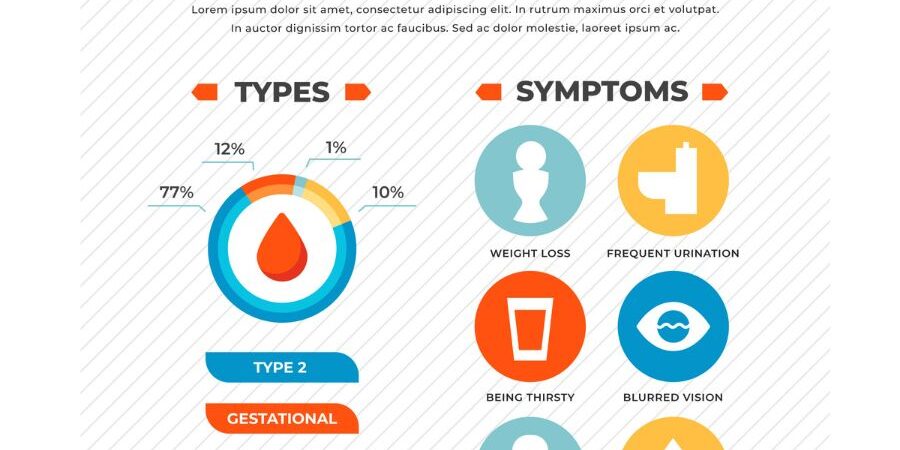
Diabetes is a chronic condition characterized by high blood sugar levels. It occurs when the body is unable to produce enough insulin or properly use the insulin it produces. There are two main types of diabetes: type 1 and type 2. While they may share some similarities, they differ in their causes, symptoms, and treatment approaches. Let’s delve into the details and explore the differences between type 1 and type 2 diabetes.
Type 1 Diabetes: Autoimmune Disorder
Type 1 diabetes, also known as insulin-dependent diabetes or juvenile diabetes, typically develops during childhood or adolescence. It is an autoimmune disorder in which the immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas. As a result, the body is unable to produce insulin, leading to high blood sugar levels.
The symptoms of type 1 diabetes often appear suddenly and include excessive thirst, frequent urination, unexplained weight loss, extreme hunger, fatigue, and blurred vision. Individuals with type 1 diabetes require lifelong insulin therapy to survive since their bodies cannot produce insulin on their own. Blood sugar monitoring, a healthy diet, regular exercise, and maintaining a healthy lifestyle are also vital in managing type 1 diabetes.
Type 2 Diabetes: Insulin Resistance
Type 2 diabetes, also known as non-insulin dependent diabetes or adult-onset diabetes, is the most common form of diabetes. It occurs when the body becomes resistant to the effects of insulin or does not produce enough insulin to maintain normal blood sugar levels. Unlike type 1 diabetes, type 2 diabetes is not an autoimmune disorder.
The risk factors for type 2 diabetes include obesity, sedentary lifestyle, family history, age, and certain ethnicities. The symptoms of type 2 diabetes may develop gradually and include frequent urination, increased thirst, fatigue, blurred vision, slow wound healing, and frequent infections. Initially, type 2 diabetes can often be managed through lifestyle modifications such as healthy eating, regular exercise, weight management, and oral medications. In some cases, insulin therapy may be necessary.
Key Differences at a Glance
To summarize the differences between type 1 and type 2 diabetes, consider the following:
Causes:
Type 1 diabetes: Autoimmune disorder leading to the destruction of insulin-producing cells.
Type 2 diabetes: Insulin resistance and/or inadequate insulin production.
Age of Onset:
Type 1 diabetes: Usually develops during childhood or adolescence.
Type 2 diabetes: Typically occurs in adulthood, but is increasingly seen in younger individuals.
Treatment:
Type 1 diabetes: Insulin therapy is required.
Type 2 diabetes: Lifestyle modifications, oral medications, and sometimes insulin therapy.
Risk Factors
Type 1 diabetes: Family history and genetic predisposition.
Type 2 diabetes: Obesity, sedentary lifestyle, family history, age, and certain ethnicities.
Prevention
Type 1 diabetes: No known prevention methods.
Type 2 diabetes: Regular physical activity, healthy eating, weight management, and avoiding tobacco and excessive alcohol consumption.
Conclusion
While both type 1 and type 2 diabetes affect blood sugar regulation, they have distinct causes, symptoms, and treatment approaches. Type 1 diabetes is an autoimmune disorder that requires lifelong insulin therapy, while type 2 diabetes is often managed through lifestyle modifications and oral medications. Understanding the differences between these two types of diabetes is crucial for individuals diagnosed with the condition and their loved ones. Remember to consult with a healthcare professional or your primary care physician for personalized advice and guidance regarding the management of diabetes.